Surgery with quicker recovery
Today's laparoscopic methods means less pain and scarring, fewer risks, and a quicker return to everyday activities.
Colon surgery traditionally has been performed through an eight- to 12-inch incision, allowing surgeons to work inside the opening to re- move a portion of the diseased bowel and reconnect the two remaining sections.
With laparoscopic surgery, a large “open” incision no longer is needed. Instead, surgeons operate through several small incisions—each about one-quarter-inch long—through which they insert the laparoscope and special instruments to perform the same procedure.
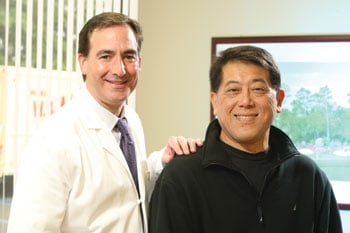
For patients like George Houng, this minimally inva- sive technique meant less pain and scarring, a shorter hospital stay and quicker recovery. Within several weeks, the 55-year-old accountant was able to return to normal activities, including work.
“The advanced visualization capabilities of the laparoscope give us a better view than seeing the surgical site with the naked eye,” explains board-certified colorectal surgeon Roy Dressner, D.O. “We are able to watch the enlarged image of the patient’s internal organs on a television monitor as we perform the procedure through the small openings.”
Since laparoscopic colectomy was introduced in 2001, Dr. Dressner and his colleagues at Monmouth Medi- cal Center have performed more than 1,000 procedures. Monmouth has the lowest conversion rate from laparo- scopic to open colorectal surgery in the region—4 percent vs. 15 percent nationally. The hospital also was the first in the New Jersey invited to broadcast live laparoscopic colon surgery to a meeting of the American College of Surgeons.
“This procedure is proving extremely effective in treating colon cancer, benign polyps and diverticulitis, as well as other diseases of the colon,” Dr. Dressner says. “Because of our experience in this sophisticated technique, a growing number of patients are becoming candidates for the procedure, reducing their risk for complications that can result from open surgery.”
Specifically, patients undergoing laparoscopic colectomy are less likely to lose a large amount of blood, or develop wound infections or abdominal hernia.
“I feel good, and my recovery went very well,” says Houng, a resident of Eatontown whose surger y was done at Monmouth last September by Dr. Dressner. “I had almost a foot of my colon removed. Now that my colon is shorter, I know I need to eat smaller meals."
“I was on a liquid diet at first, but now I have a normal diet,” he adds. “I ate well, rested, and got my strength back.”
Initially diagnosed in July of 2009 when a routine colonoscopy revealed a number of cancerous polyps, he is followed every two months by Dr. Dressner. With a family history of the disease, the father of three (ages 22, 18 and 14) notes that he will encourage his children to be followed closely for the disease, which is highly preventable and curable if caught early.
“My father was diagnosed with colon cancer at 70—he had the surgery too, and is doing well now at 81,” he says.
Dr. Dressner points to enrollment in the Familial Colorectal Cancer Registry Program at Monmouth as an- other key to cancer survivorship. In conjunction with the High-Risk Cancer Assessment Program at the Leon Hess Cancer Center, the Registry Program offers a multi-specialty team approach to the assessment of family risk, genetic coun- seling and testing and treatment of polyps and cancer. The registry promotes knowledge of the risks and implication of a family history of colorectal cancer. A geneticist provides patients with education about the disease, tests, surgical options, lifelong surveillance protocols and genetic testing.